|
Hernia Surgery
 Approximately 80,000 inguinal hernia repair operations are performed annually in the United Kingdom. Many are performed by the conventional "open" method. Some are performed laparoscopically. Laparoscopic hernia repair is a relatively new surgical technique to fix tears in the abdominal wall (muscle) using small incisions, a patch (mesh), and special cameras to view inside the body. It offers a more rapid recovery for the patient, less postoperative pain, and a quicker return to work and normal activities. Approximately 80,000 inguinal hernia repair operations are performed annually in the United Kingdom. Many are performed by the conventional "open" method. Some are performed laparoscopically. Laparoscopic hernia repair is a relatively new surgical technique to fix tears in the abdominal wall (muscle) using small incisions, a patch (mesh), and special cameras to view inside the body. It offers a more rapid recovery for the patient, less postoperative pain, and a quicker return to work and normal activities.
What is a Hernia?
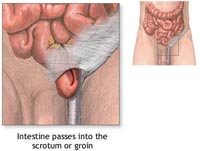
 A hernia is a defect in the abdominal wall, in which the inside layers of the abdominal muscle have weakened resulting in a bulge or tear. When a loop of intestine or abdominal tissue pushes through the defect, severe pain and other potentially serious complications can result. A hernia is a defect in the abdominal wall, in which the inside layers of the abdominal muscle have weakened resulting in a bulge or tear. When a loop of intestine or abdominal tissue pushes through the defect, severe pain and other potentially serious complications can result.
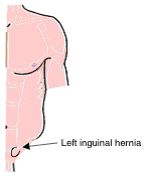 Both men and women can get a hernia. A hernia does not get better over time; a hernia will not go away by itself. There are three different types of hernia that can be repaired laparoscopically:(Left-Illustration of loops of bowel protruding through the abdominal wall) Both men and women can get a hernia. A hernia does not get better over time; a hernia will not go away by itself. There are three different types of hernia that can be repaired laparoscopically:(Left-Illustration of loops of bowel protruding through the abdominal wall)
Inguinal hernias, these are felt or seen in the groin (see diagram on left)
Incisional hernias, occuring at or near the site of a previous surgical operation
Para-umbilical hernias, seen around the belly button
How do I Know if I Have a Hernia?
 Frequently, hernias are easily felt and diagnosed. You may notice a bulge under the skin. You may feel pain when you lift heavy objects, cough, strain during urination or bowel movements or during prolonged standing or sitting. Frequently, hernias are easily felt and diagnosed. You may notice a bulge under the skin. You may feel pain when you lift heavy objects, cough, strain during urination or bowel movements or during prolonged standing or sitting.
The pain may be sharp and immediate or a dull ache that gets worse toward the end of the day. Severe, continuous pain, redness and tenderness are signs that the hernia may be entrapped or strangulated. These symptoms are cause for concern and immediate contact with you GP or local hospital.

What causes Hernias?
The wall of the abdomen has natural areas of potential weakness. Hernias can develop at these or other areas due to heavy strain on the abdominal wall, aging, injury, an old operation scar or a weakness in the abdominal wall present at birth. Anyone can get a hernia at any age. Most hernias in children are congenital. In adults, a natural weakness or strain from heavy lifting, persistent coughing, and difficulty with bowel movements or urination can cause the abdominal wall to weaken or separate, and hernias to form.
Treatment Options
There is no acceptable non-surgical medical treatment for a hernia. The use of a truss (hernia belt) can help keep the hernia from bulging but eventually will fail. The truss also causes the formation of scar tissue around the hernia making the repair more difficult. If you suspect you have a hernia, consult with your GP promptly. Delayed hernia repair can result in intestinal incarceration (intestine is trapped inside the hernia sac) or strangulation (intestine is trapped and develops gangrene). The latter is a surgical emergency.
The hernia will not go away without treatment; it will only get bigger. The bigger the defect the bigger the operation required to fix it.
Under certain circumstances the hernia may be watched and followed closely by a physician. These situations are unique to those individuals who are at high operative risks (i.e. those with severe heart or lung disease, or bleeding problems). Of course, even in the high risk person, if the symptoms become severe or if strangulation occurs, then an operation must be performed.
Laparoscopic Inguinal Hernia Repair
 In laparoscopic hernia surgery, a telescope attached to a camera is inserted through a small incision that is made under the patient's belly button. Two other small cuts are made (each no larger than the diameter of pencil) in the lower abdomen. The hernia defect is reinforced with a 'mesh' (synthetic material made from the same material that stitches are made from) and secured in position with titanium tacks. In laparoscopic hernia surgery, a telescope attached to a camera is inserted through a small incision that is made under the patient's belly button. Two other small cuts are made (each no larger than the diameter of pencil) in the lower abdomen. The hernia defect is reinforced with a 'mesh' (synthetic material made from the same material that stitches are made from) and secured in position with titanium tacks.
How do open and laparoscopic hernia repairs compare?
Both the laparoscopic and the standard open inguinal hernia repair (known as the Lichenstein repair) use a synthetic mesh which stimulates the formation of scar tissue, strengthens the area and reduces recurrence rates.
Type of Anaestheric: Inguinal hernias can be repaired by either the open or laparoscopic approach under general anaesthetic (GA). If a patient is not fit to have a GA then it can be repaired by the open method under local anaesthetic.
Post-operative pain: Patients experience significantly less pain, or require fewer painkillers, immediately after a laparoscopic hernia repair compared to an open procedure.
Return to work: After laparoscopic hernia repair motivated patients will be able to return to work after 2 or 3 days. For an open procedure fitness to return to work will take considerably longer.
Long term pain or numbness: A recent study showed that five years after open hernia repair 10% of patients still experienced groin pain and 22% reported parasthesia (numbness) in the groin. This compares with significantly less patients who experienced these symptoms following laparoscopic repair (2% and 2.5% respectively)
The difference between the two types of procedure is most likely due to the close proximity of nerves in the operating field during open hernia repairs. These nerves are further away from the area being operated upon in laparoscopic surgery.
Recurrence rate : Both open and laparoscopic hernia repairs have very low chances of recurrence, with no difference between the procedures.

What are the government guidelines on laparoscopic hernia surgery?
The National Institute of Clinical Excellence (NICE), a government body with responsibility to advise on best and most effective treatments, have recently recommended that laparoscopic hernia surgery should be considered if the surgeon is fully trained in this type of surgery. Patients with recurrent or bilateral (both sides) hernias as well as those with primary hernias can be offered laparoscopic repair.
Laparoscopic Incisional Hernia Repair
An incisional hernia is a defect in the abdominal wall through the site of an old operation scar. Incisional hernias form after surgery through the incision site or previous drain sites, or laparoscopic trocar insertion sites. Incisional hernias are reported to occur in approximately 4-10% of patients after open surgical procedures. Certain risk factors predispose patients to develop Incisional hernias, such as obesity, diabetes, respiratory disease, steroids, postoperative wound infection and smoking, as well as poor surgical technique. Approximately 25,000 incisional hernia repairs are performed annually in the United Kingdom .
These hernias present much the same way inguinal hernias do. That is, they present with a bulge near or at a previous incision. Some patients may experience discomfort, abdominal cramping or complete intestinal obstruction, or incarceration as a result of these hernias.
The principle of surgical repair entails the use of prosthetic mesh to repair large defects in order to minimize tension on the repair. A tension free repair has a lesser chance of hernia recurrence. Traditionally, the old scar is incised and removed, and the entire length of the incision inspected. Generally, there are multiple hernia defects other than the one(s) discovered by physical examination. The area requiring coverage is usually large and requires much surgical dissection. A prosthetic mesh is used to cover the defect(s), and the wound closed. This is a major surgical procedure and often complicated. Infection rates following repair may be as high a 7.0%. Recurrence of the hernia after open repair can be up to 5%, or higher, depending on the patient's preoperative risk factors.
The laparoscopic repair of incisional hernias was designed to minimise operative trauma to the patient. As mentioned, these are often complicated repairs requiring large incisions and extensive tissue dissection. A large piece of prosthetic mesh is placed under the hernia defect with a wide margin of mesh outside the defect. The mesh is secured to the anterior abdominal wall with a varying number of tacs, placed laparoscopically.
A patient is a candidate for laparoscopic incisional hernia repair if they are medically able to undergo general anesthesia. Also, the defect must allow the surgeon to place the laparoscopic trocars in such positions that repair are ergonomically possible. In some very large or giant hernias, the abdominal wall is distorted to such a degree that it is impossible to safely place laparoscopic trocars.
Patients are admitted the same day of their surgery. Following the procedure and recovery from anesthesia, they are taken to the ward where they spend the night. We encourage our patients to move as quickly as possible. It is extremely important to be active early in order to stave off some of the complication seen postoperatively, such as pneumonia, deep venous thrombosis and pulmonary embolism (clots in the legs that break off and go the lungs). Postoperative pain is variable, and can be considerable during the first 24 hours. As such, patients are given I.V. narcotics as needed, and are changed to oral analgesics the next day. Generally, most patients stay in the hospital 1 or 3 days following surgery. There is no dietary restriction. Activity level is restricted by the patient's comfort level. However, it is generally not advisable to engage in any strenuous exercise or heavy lifting for 2-3 weeks after surgery to allow the hernia repair to heal.

Risks of Laparoscopic Hernia Surgery
Any operation may be associated with complications. The primary complications of any operation are bleeding and infection, which are uncommon with laparoscopic hernia repair.
There is a slight risk of injury to the urinary bladder, the intestines, blood vessels, nerves or the sperm tube going to the testicle.
Difficulty urinating after surgery is not unusual and may require a temporary tube into the urinary bladder.
Any time a hernia is repaired it can come back. Recurrence rate is 1%. Your surgeon will help you decide if the risks of laparoscopic hernia repair are less than the risks of leaving the condition untreated.
What Preparation is Required for Surgery?
Most hernia operations are performed on an outpatient basis, meaning the patient will go home on the same day that the operation is performed.
You should refrain from eating or drinking after midnight on the night before your operation.
You should shower the night before or the morning of the operation.
If you have difficulties moving your bowels, an enema or similar preparation should be used after consulting with your surgeon.
Some preoperative testing may be required depending on your medical condition and the type of anesthesia needed for your operation.
If you take medication on a daily basis, discuss this with your surgeon as he may want you to take some of your medications on the morning of surgery with a sip of water. If you take aspirin, blood thinners or arthritis

What Should I Expect After Surgery?
Following the operation, you will be transferred to the recovery room where you will be monitored carefully until you are fully awake.
Once you are awake and able to walk, you will be discharged.
With any hernia operation, you can expect some soreness. This will be mostly during the first 24 to 48 hours.
You are encouraged to be up and about the day after surgery.
If you begin to have fever, chills, vomiting, are unable to urinate, or experience drainage from your incisions, you should call your surgeon immediately.
With laparoscopic hernia repair, you will probably be able to get back to your normal activities within a short amount of time. These activities include showering, driving, walking up stairs, lifting, work and sexual intercourse.
If you have prolonged soreness and are getting no relief from the prescribed pain medication, you should notify your surgeon. You should call and schedule a follow-up appointment within 2 weeks after you operation.
Wounds should be kept dry for 5 days after surgery

|